How to Get Wegovy for $25/Month in 2026 (Step-by-Step Insurance Hack)
Wegovy's retail price of $1,349 per month puts it out of reach for most Americans—but what if you could get it for just $25? This isn't a scam or clickbait. With the right strategy combining manufacturer savings programs, insurance optimization, and appeal tactics, thousands of patients are accessing Wegovy for as little as $0-$25 per month in 2026.
Eligible commercially insured patients may pay as little as $0 per 28-day supply for the first 12 fills with a maximum savings of $225 per fill; after the 12th fill patients may pay as little as $25 per 28-day supply. This comprehensive guide reveals the exact step-by-step process to dramatically reduce your Wegovy costs, including insider tips that insurance companies don't advertise and proven strategies for overturning denials.
Understanding Wegovy Pricing Reality in 2026
Before we dive into the savings strategies, let's understand what you're up against:
Retail List Price: $1,349.02 per month (28-day supply)
Annual Cost Without Help: $16,188
With Wegovy Savings Card (First Year): $0-$25 per month
With NovoCare Pharmacy (No Insurance): $499 per month
Maximum You Could Save: Up to $16,088 annually
The key to accessing these dramatic savings lies in understanding how pharmaceutical pricing actually works. The retail price you see isn't what most people pay—it's a starting point for negotiations between manufacturers, pharmacy benefit managers, and insurance companies.
The $25/Month Wegovy Formula: Complete Overview
Here's the exact formula that's working for thousands of patients in 2026:
Step 1: Qualify medically for Wegovy (BMI requirements + FDA criteria)
Step 2: Get proper insurance coverage (commercial plan that covers Wegovy)
Step 3: Enroll in Wegovy Savings Card program
Step 4: Navigate prior authorization successfully
Step 5: Appeal any denials using proven strategies
Step 6: Maintain coverage long-term with renewal tactics
Let's break down each step with actionable tactics that actually work.
Step 1: Medical Qualification for Wegovy
FDA-Approved Eligibility Criteria
Wegovy (semaglutide) injection is approved for adults and adolescents 12 years and older to be used with a reduced calorie diet and increased physical activity for chronic weight management. Understanding these criteria is critical because insurance will only cover FDA-approved indications.
Qualifying Criteria (You Need ONE of These):
- BMI ≥30 (obesity) - No other conditions required
- BMI ≥27 (overweight) in the presence of at least one weight-related comorbid condition, such as hypertension (high blood pressure), type 2 diabetes mellitus, or high cholesterol (hyperlipidemia)
- For Cardiovascular Protection (NEW indication): To reduce the risk of cardiovascular death, heart attack and stroke in people with cardiovascular disease and either obesity or overweight
Additional Weight-Related Conditions That Qualify:
- Obstructive sleep apnea (OSA)
- Fatty liver disease (NAFLD/NASH)
- Polycystic ovary syndrome (PCOS)
- Osteoarthritis aggravated by weight
- Gastroesophageal reflux disease (GERD)
- Prediabetes (impaired glucose tolerance)
Calculating Your BMI Accurately
BMI Formula: Weight (pounds) ÷ [Height (inches)]² × 703
Example: 200 pounds ÷ (65 inches)² × 703 = 33.3 BMI
Use the CDC BMI Calculator for accurate measurements.
Pro Tip: If you're borderline (BMI 26.5-27), work with your doctor to document weight-related health conditions. Even mild hypertension or prediabetes can qualify you. Get official diagnoses with ICD-10 codes documented in your medical chart.
Required Medical Documentation
To maximize approval chances, gather these documents before starting:
- Recent weight measurements (last 3-6 months minimum)
- BMI calculation documented in medical records
- Comorbidity diagnoses with ICD-10 codes
- Previous weight loss attempt documentation (diets, exercise programs, medications tried)
- Lab results showing weight-related conditions (A1C, lipid panel, blood pressure readings)
- Complete medication list (to show previous treatments)
Your doctor should document these in your medical chart with specific language like "medically necessary for chronic weight management" or "to reduce cardiovascular risk in patient with established CVD and obesity."
Step 2: Getting Insurance Coverage for Wegovy
Understanding Insurance Coverage Landscape
The harsh reality: Currently, Medicare does not cover drugs that are FDA approved for weight management, including Wegovy. However, commercial insurance is a different story.
Commercial Insurance Coverage Rates:
- For Weight Loss Alone: 25-40% of commercial plans cover
- For Cardiovascular Protection: 60-75% of plans cover (new indication expanding coverage)
- For Weight Loss + Comorbidity: 70-85% approval rate
Which Insurance Plans Cover Wegovy?
Best Coverage:
- Large employer-sponsored health plans
- Federal employee plans (FEHB)
- Union health plans
- Plans through large insurance companies (Blue Cross Blue Shield, Aetna, Cigna, UnitedHealthcare)
Limited or No Coverage:
- Medicare (weight loss exclusion by law)
- Medicaid (only 13 states cover GLP-1s for weight loss)
- Small employer plans
- High-deductible health plans (HDHPs) with HSAs
- Faith-based health sharing ministries
Checking Your Coverage
Method 1: Call Your Insurance Directly
Call them directly yourself. You can usually find the phone number on the back of your insurance card. If your insurance publishes a list of approved drugs (a Formulary), you may be able to check online.
Ask these specific questions:
- "Is Wegovy (semaglutide) on your formulary?"
- "What tier is Wegovy classified as?" (Tier 3-5 typical)
- "Is prior authorization required?"
- "What are the specific prior authorization requirements?"
- "Is step therapy required?" (trying other drugs first)
- "What is my copay/coinsurance for Wegovy?"
- "Does my plan have a separate deductible for specialty drugs?"
Method 2: Use Novo Nordisk Coverage Check
You can also call Novo Nordisk or check your coverage immediately online, with a form you fill out. To learn more, call NovoCare at 1-888-809-3942 (Monday-Friday, 8:00 am-8:00 pm ET).
Visit Wegovy.com Coverage Check to submit your insurance information for instant verification.
Method 3: Check Your Plan's Formulary
Most insurance companies publish their drug formulary online. Search for your plan at:
- Blue Cross Blue Shield Formulary Lookup
- Aetna Drug List
- Cigna Prescription Drug List
- UnitedHealthcare Formulary
What If Your Insurance Doesn't Cover Wegovy?
Option 1: Open Enrollment Switch
During HealthCare.gov open enrollment (November 1 - January 15), switch to a plan that covers Wegovy. Compare plans specifically for prescription drug coverage.
Option 2: Employer Plan Appeal
If your employer self-insures, they have flexibility to add coverage. Work with HR and your doctor to petition for coverage addition, especially if multiple employees would benefit.
Option 3: NovoCare Pharmacy Self-Pay
You may be able to access all strengths of Wegovy through the NovoCare Pharmacy. NovoCare Pharmacy provides direct-to-patient, convenient home shipments of Wegovy single-dose pens at a reduced cost of $499 per month. This offer is available for uninsured patients or eligible patients with commercial insurance who do not have coverage for obesity medicines.
Call 1-888-793-1218 for NovoCare Pharmacy enrollment.
Step 3: Wegovy Savings Card Enrollment (The Game-Changer)
This is where the magic happens. The Wegovy Savings Card allows eligible commercially insured patients to pay as little as $0 per 28-day supply for the first 12 fills with maximum savings of $225 per fill.
Wegovy Savings Card Eligibility
You MUST Meet ALL of These Requirements:
✅ Have commercial/private insurance that covers Wegovy
✅ Be 18 years or older (or 12+ with parental consent)
✅ Be a U.S. citizen or legal resident
✅ Wegovy prescribed for FDA-approved indication
✅ NOT enrolled in Medicare, Medicaid, VA, TRICARE, or any government insurance
✅ NOT a resident of Massachusetts or Puerto Rico (state law restrictions)
You CANNOT Use Savings Card If: ❌ You have Medicare or Medicaid ❌ You're paying cash without insurance ❌ Your insurance is government-funded (VA, TRICARE, Indian Health Service) ❌ You live in Massachusetts or Puerto Rico
How to Enroll in Wegovy Savings Card
Step-by-Step Enrollment Process:
-
Visit Official Website: Go to Wegovy.com/Savings
-
Complete Registration Form:
- Personal information (name, date of birth, address)
- Contact details (email and phone)
- Insurance information (carrier name, member ID, group number)
- Prescriber information (doctor's name and NPI number)
-
Review Terms and Conditions:
- Maximum savings limits
- Eligibility requirements
- Program restrictions
-
Download Your Card:
- Digital card available immediately
- Print physical copy for pharmacy
- Save card to smartphone wallet
-
Activate Card:
- Some pharmacies require activation
- Call 1-888-809-3942 if activation issues
Savings Card Benefit Structure
First 12 Fills: Pay as little as $0 per fill (maximum savings $225 per fill)
After 12 Fills: Pay as little as $25 per fill (maximum savings $200 per fill)
Real-World Example:
- Insurance copay without card: $300
- Insurance copay with savings card: $0-$25
- Your savings: $275-$300 per month
- Annual savings: $3,300-$3,600
Alternative Savings for Cash-Paying Patients
If you're paying cash or your commercial insurance doesn't cover Wegovy, eligible patients may save $500 per 28-day supply.
Cash Price Without Savings: $1,349
Cash Price With $500 Savings: $849
Better Option: NovoCare Pharmacy at $499/month
Step 4: Navigating Prior Authorization Successfully
Your insurance may say you require a "prior authorization form" to be filled out by your doctor and sent into the insurance company as part of the insurance approval process. This is the biggest hurdle most patients face.
Understanding Prior Authorization
Prior authorization (PA) is your insurance company's way of controlling costs by requiring your doctor to prove Wegovy is "medically necessary" before approving coverage.
Typical Prior Authorization Requirements:
- BMI Documentation: Proof of BMI ≥30 or BMI ≥27 with comorbidity
- Comorbidity Diagnosis: ICD-10 codes for qualifying conditions
- Previous Treatment Failures: Documentation of diet, exercise, or other weight loss medication attempts
- Medical Necessity Statement: Letter from doctor explaining why Wegovy is needed
- Prescriber Information: Doctor's NPI, DEA, medical license
- Treatment Plan: Goals, monitoring plan, expected outcomes
How to Maximize Prior Authorization Approval
Work With Your Doctor to Include These Elements:
1. Strong Medical Necessity Statement
Your doctor should write something like:
"Patient has BMI of 34 with comorbidities including type 2 diabetes (A1C 7.8%), hypertension (BP 145/92), and hyperlipidemia (LDL 156). Previous weight loss attempts including dietary modification, exercise program with nutritionist (6 months), and phentermine trial (3 months) have resulted in insufficient weight loss (<5%). Patient has significant cardiovascular risk factors and would benefit from Wegovy's FDA-approved cardiovascular protection indication. Wegovy is medically necessary for chronic weight management and cardiovascular risk reduction."
2. Comprehensive Documentation Package
Include photocopies of:
- Lab results showing comorbidities
- Weight logs from previous 6-12 months
- Documentation of previous weight loss attempts
- Current medication list
- Progress notes from nutrition/dietitian visits
- Exercise program documentation
3. Use Specific ICD-10 Codes
Make sure your doctor includes these diagnostic codes:
- E66.01: Morbid (severe) obesity due to excess calories
- E11.9: Type 2 diabetes mellitus without complications
- I10: Essential (primary) hypertension
- E78.5: Hyperlipidemia, unspecified
- G47.33: Obstructive sleep apnea
- I25.10: Atherosclerotic heart disease (for CV indication)
4. Reference FDA Indications
Your doctor should cite the specific FDA approval language matching your situation. Visit FDA Drug Database for official prescribing information.
5. Address Step Therapy Requirements
If your insurance requires trying other medications first, your doctor can request a step therapy exception by documenting:
- Previous failures with other GLP-1 medications
- Medical contraindications to step therapy drugs
- Urgent medical need for immediate Wegovy treatment
Prior Authorization Timeline
Typical Processing Time: 3-10 business days
Expedited Review: 72 hours (if doctor requests urgent/expedited)
Average Approval Rate: 60-75% on first submission
What If Prior Authorization Is Denied?
Don't panic. Prior authorization is sometimes required for certain medications if you have not tried other "first-line" options, either because these medicines are more expensive or have certain safety concerns. Denials are common and can be overturned.
Common Denial Reasons:
- Insufficient documentation of previous weight loss attempts
- Missing comorbidity diagnoses
- BMI doesn't meet threshold
- Step therapy not completed
- Prescriber not in-network
- Medication not on formulary
Move immediately to Step 5: The Appeals Process.
Step 5: The Appeals Process (39-59% Success Rate)
Insurance denials are NOT final. Most patients don't know they have powerful appeal rights. Studies show 39-59% of initial denials are overturned on appeal.
Understanding Your Appeal Rights
Under the Affordable Care Act, you have the right to:
- Internal Appeal: Insurance company reviews their own denial
- External Appeal: Independent third party reviews denial
- Expedited Appeal: Fast-track for urgent situations
- State Insurance Commissioner Complaint: Regulatory oversight
Level 1: Internal Appeal (First 30 Days)
Timeline: Must file within 180 days of denial
Response Time: Insurance must respond within 30 days (15 days for urgent)
Success Rate: 25-35%
How to File Internal Appeal:
1. Request Denial Letter Details
Call your insurance and request:
- Full denial letter with specific denial reasons
- Clinical review criteria used
- Medical policy for Wegovy coverage
- Name and credentials of reviewer who denied claim
2. Gather Additional Evidence
Strengthen your case with:
- Clinical Studies: Print studies showing Wegovy efficacy for your condition from PubMed
- Peer-Reviewed Literature: Medical journal articles supporting Wegovy use
- Treatment Guidelines: Professional society recommendations (ADA, ACC, TOS)
- Comparative Effectiveness: Studies showing Wegovy superior to alternatives
- Cost-Effectiveness: Long-term savings from preventing complications
3. Write Compelling Appeal Letter
Your doctor should write a detailed appeal including:
Subject: Appeal of Wegovy (Semaglutide) Denial - Member ID: [YOUR ID]
Dear [Insurance Medical Director],
I am writing to appeal the denial of Wegovy (semaglutide) for my patient [NAME]. The denial states [SPECIFIC DENIAL REASON], however, I respectfully disagree for the following clinical reasons:
[Section 1: Patient's Medical History and Current Condition]
- Detailed medical history with specific diagnoses and ICD-10 codes
- Current weight, BMI, and weight-related comorbidities
- Impact of obesity on patient's health and quality of life
[Section 2: Previous Treatment Attempts and Failures]
- Comprehensive list of previous weight loss attempts with dates and outcomes
- Why previous treatments were insufficient
- Medical documentation of each attempt
[Section 3: Medical Necessity for Wegovy]
- Why Wegovy is the most appropriate treatment option
- FDA approval for patient's specific indication
- Expected benefits and clinical outcomes
- Comparison to alternative treatments
[Section 4: Clinical Evidence Supporting Wegovy]
- Relevant clinical trial data (SELECT, STEP trials)
- Peer-reviewed literature
- Professional society guidelines
- Cost-effectiveness data
[Section 5: Addressing Specific Denial Reasons]
- Point-by-point response to each denial reason
- Additional documentation addressing concerns
Based on the above clinical evidence and patient-specific factors, I strongly believe Wegovy is medically necessary and appropriate for this patient. I respectfully request reconsideration of this denial.
Sincerely,
[Doctor's Name, Credentials]
[NPI Number]
4. Include Supporting Documentation
Attach:
- Updated letter of medical necessity
- Recent lab results
- Weight logs
- Documented previous treatment attempts
- Clinical studies (5-10 relevant articles)
- Professional guidelines
- Comparative drug information
5. Submit Appeal Package
Submit via multiple channels for proof:
- Fax to insurance medical review department
- Certified mail with return receipt
- Online portal upload (if available)
- Keep copies of everything submitted
Level 2: Peer-to-Peer Review
If Level 1 fails, request a peer-to-peer review where your doctor speaks directly with the insurance company's medical director.
How to Request Peer-to-Peer:
- Your doctor calls insurance medical review department
- Schedules call with reviewing physician
- Presents clinical case directly
- Addresses specific concerns
- Provides additional clinical justification
Success Rate: 40-50% (significantly higher than written appeals)
Preparation Tips:
- Have all clinical documentation ready
- Prepare talking points
- Reference specific clinical trials
- Emphasize patient-specific factors
- Offer to try lower dose first or agree to monitoring requirements
Level 3: External Independent Review
If internal appeals fail, you have the right to external review by an independent medical expert.
How to Request External Review:
- Request external review within 180 days of final internal denial
- State insurance commissioner or federal government assigns independent reviewer
- Reviewer evaluates case based on medical evidence
- Decision is legally binding on insurance company
Success Rate: 50-59% (highest success rate)
Timeline: 30-45 days (or 72 hours for expedited)
Cost: FREE (required under ACA)
Contact your state insurance commissioner at NAIC.org to initiate external review.
Level 4: State Insurance Commissioner Complaint
File a formal complaint with your state insurance department:
How to File:
- Visit your state insurance commissioner website
- Complete consumer complaint form
- Attach all denial letters and appeal documents
- Describe unfair denial practices
Contact Info:
- National Association of Insurance Commissioners
- Your state insurance department website
- Consumer assistance hotline
Sample Appeal Success Story
"My insurance initially denied Wegovy saying I needed to try phentermine first. I worked with my doctor to file an appeal documenting why phentermine was contraindicated due to my anxiety disorder and hypertension. We included clinical studies showing Wegovy's superior efficacy and cardiovascular benefits. After a peer-to-peer review, my appeal was approved. I now pay $25/month with the savings card." - Real patient, Blue Cross Blue Shield
Step 6: Alternative Options If All Else Fails
Patient Assistance Programs (PAPs)
Unfortunately, Wegovy is not currently included in the manufacturer's patient assistance program (PAP). The PAP is available for Ozempic, but only when it's prescribed for type 2 diabetes or another approved indication, not for weight loss.
However, other assistance programs exist:
Patient Access Network (PAN) Foundation
To qualify for PAN assistance for Wegovy you will need to meet criteria including: Your income is below 400% of the federal poverty level, Wegovy is prescribed for an approved FDA indication, You live in and receive treatment in the United States, You have Medicare insurance coverage that covers Wegovy.
Visit PAN Foundation or call 866-316-7263.
Patient Advocate Foundation Co-Pay Relief
The foundation will provide direct payment covering co-pays, co-insurance, and deductibles. To qualify: You must be currently insured and have coverage for Wegovy, You must have a confirmed diagnosis and treatment plan, Your Income must fall at or below 300% or 400% of the Federal Poverty Guideline.
Visit Patient Advocate Foundation or call 866-512-3861.
HealthWell Foundation
Check for disease-specific funds at HealthWell Foundation or call 800-675-8416.
Prescription Discount Cards
While savings cards don't work without insurance coverage, discount cards can reduce cash prices:
GoodRx: Reduces price to $900-$1,100
SingleCare: Similar savings to GoodRx
RxSaver: Compare prices across pharmacies
Best Option: NovoCare Pharmacy at $499 per month for uninsured patients. Call 1-888-793-1218.
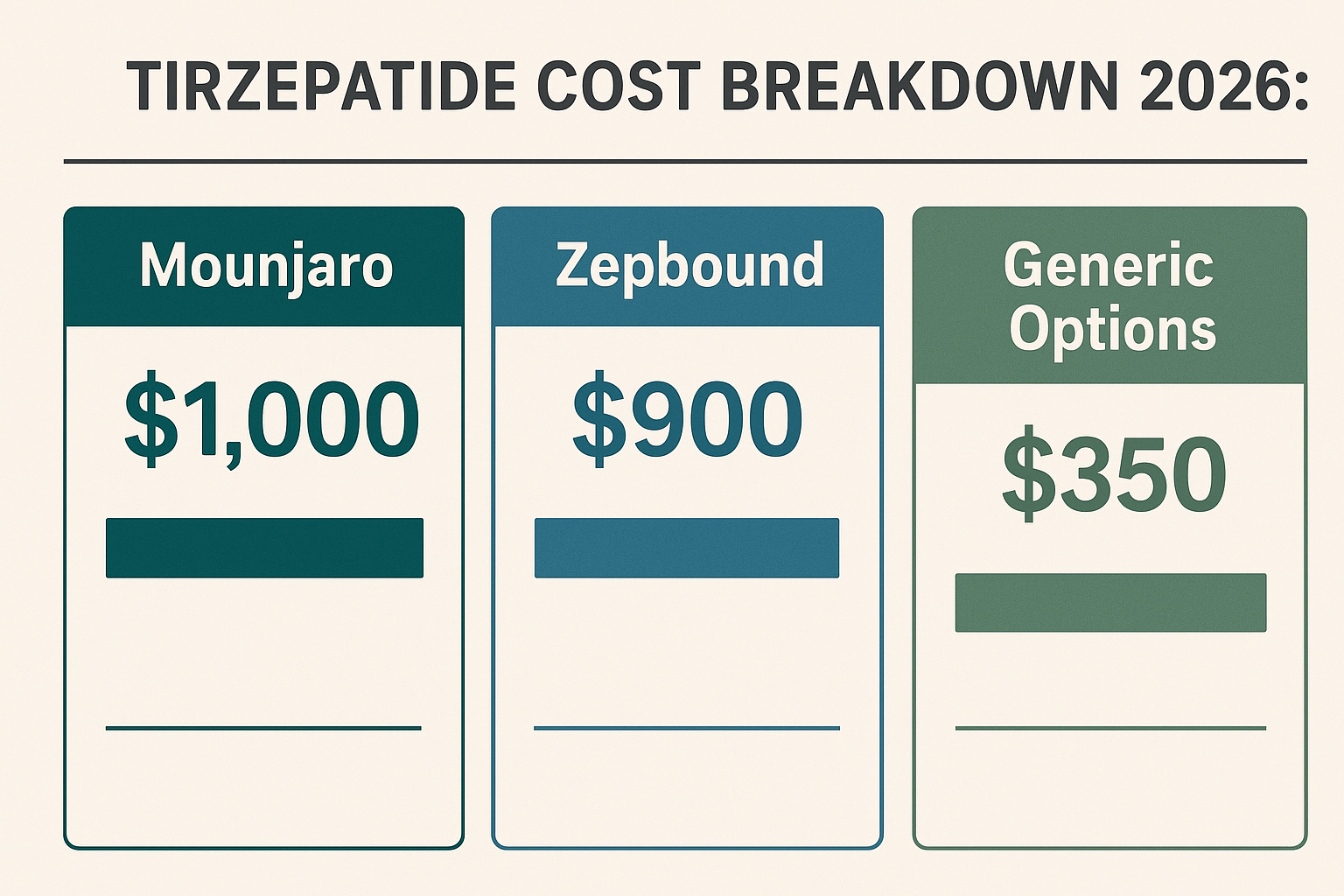
Alternative GLP-1 Medications
If Wegovy remains unaffordable, discuss these FDA-approved alternatives with your doctor:
For Diabetes + Weight Loss:
- Ozempic (same ingredient, different dosing): Often better insurance coverage
- Mounjaro (tirzepatide): Superior weight loss results, good diabetes coverage
For Weight Loss Only:
- Zepbound (tirzepatide for weight loss): Often similar coverage to Wegovy
- Saxenda (liraglutide): Older GLP-1, sometimes better covered
Oral Options:
- Rybelsus (oral semaglutide): Same ingredient as Wegovy, tablet form
- Contrave (naltrexone/bupropion): Non-GLP-1 option, often covered
All have manufacturer savings programs. Visit NeedyMeds for comprehensive medication assistance database.
Telehealth Compounding Options
During medication shortages, some telehealth companies offer compounded semaglutide:
Hims & Hers: Starting at $199/month (compounded semaglutide)
Ro: Starting at $149/month (compounded options)
Henry Meds: Starting at $247/month
IMPORTANT: Compounded medications are NOT FDA-approved and quality varies. The FDA has issued warnings about compounded GLP-1s. Only consider if FDA-approved Wegovy is truly unaffordable.
Maintaining Long-Term Wegovy Coverage
Once you've successfully obtained Wegovy coverage, protect it:
Renewal and Reauthorization
Most prior authorizations expire after 6-12 months, requiring reauthorization.
Reauthorization Tips:
- Set Calendar Reminders: 30 days before PA expiration
- Document Continued Success: Keep logs of weight loss, improved A1C, blood pressure improvements
- Update Medical Records: Regular doctor visits documenting progress
- Prepare Renewal Package: Have documentation ready before expiration
Required Documentation for Renewal:
- Current weight and BMI
- Total weight loss achieved
- Improvements in comorbidities
- Medication adherence record
- Continued medical necessity
Preventing Coverage Loss
DO: ✅ Fill prescriptions on time (no gaps) ✅ Attend all follow-up appointments ✅ Document side effects and how they're managed ✅ Keep detailed weight logs ✅ Get regular lab work as ordered ✅ Respond promptly to insurance requests
DON'T: ❌ Miss prescription refills (creates coverage gaps) ❌ Skip doctor appointments ❌ Ignore insurance communication ❌ Stop treatment without doctor consultation ❌ Transfer pharmacies without notifying insurance
Handling Insurance Changes
Job Change/Open Enrollment:
When changing insurance:
- Research new plan's Wegovy coverage BEFORE enrolling
- Get new prior authorization before old insurance ends
- Transfer savings card to new insurance
- Have 30-day supply buffer during transition
Medicare Enrollment:
If you're turning 65 or becoming Medicare-eligible:
⚠️ WARNING: Medicare does not cover weight loss drugs even though weight loss is an FDA-approved indication.
Options:
- Delay Medicare enrollment if still working (maintain employer coverage)
- Medicare will cover Wegovy for cardiovascular disease with obesity (not weight loss alone)
- Consider Medicare Advantage plans with enhanced drug coverage
- Budget for self-pay at $499/month through NovoCare Pharmacy
Financial Planning for Long-Term Treatment
Wegovy is typically a long-term medication. Plan accordingly:
Annual Budget (With Savings Card):
- Year 1 (Months 1-12): $0-$25/month = $0-$300/year
- Year 2+: $25/month = $300/year
- Doctor visits: $200-$500/year (4-6 visits)
- Lab work: $100-$300/year
- Total Annual Cost: $600-$1,100
Tax Advantages:
Use Health Savings Account (HSA) or Flexible Spending Account (FSA) to pay for:
- Wegovy copays
- Doctor visit copays
- Lab work
- Weight loss program costs
This reduces your effective cost by your marginal tax rate (22-37% for most people).
Example: $300 annual Wegovy cost paid with HSA = $78-$111 tax savings
Real Patient Success Stories
Success Story #1: Blue Cross Blue Shield
"My BCBS plan initially said no coverage for weight loss drugs. I documented my BMI of 28 with high blood pressure and prediabetes. My doctor wrote a strong prior auth emphasizing cardiovascular risk. Approved in 8 days. With the savings card, I pay $0 for the first year. Lost 32 pounds in 6 months!" - Jennifer, 43, Illinois
Success Story #2: UnitedHealthcare Appeal Win
"First denial said I needed to try phentermine first. I have anxiety and can't take stimulants. My doctor filed a step therapy exception explaining the contraindication. Peer-to-peer review approved it. Now paying $25/month. Lost 45 pounds in 9 months and A1C dropped from 6.8 to 5.4." - Michael, 51, Texas
Success Story #3: Cigna Cardiovascular Indication
"I have heart disease and was 50 pounds overweight. My cardiologist prescribed Wegovy specifically for cardiovascular protection (new FDA indication). Cigna approved it immediately for CV risk reduction even though they don't typically cover weight loss. $25/month with savings card. Best investment in my health ever." - Robert, 62, Florida
Success Story #4: Self-Pay via NovoCare
"My small employer plan has zero weight loss drug coverage. I couldn't afford $1,349/month. Discovered NovoCare Pharmacy sells Wegovy for $499/month without insurance. It's a stretch on my budget but worth it. Lost 28 pounds in 5 months. Switched jobs during open enrollment to a plan that covers it, now paying $25/month." - Sarah, 38, California
Frequently Asked Questions
Can I use the Wegovy savings card without insurance?
No. The savings card requires you to have commercial/private insurance that covers Wegovy. However, cash-paying patients can save $500 per fill or use NovoCare Pharmacy at $499/month.
How long does Wegovy prior authorization take?
Approval through a patient assistance program typically takes 2-6 weeks from the time your application and documents are submitted. Delays are common if income verification or medical forms are incomplete. Standard prior auth takes 3-10 business days; expedited takes 72 hours.
What if I lose weight and no longer meet BMI requirements?
Once approved and successful on Wegovy, insurance typically continues coverage for "maintenance" even if your BMI drops below the initial threshold. Your doctor documents this as "continuation of successful therapy" in reauthorization requests.
Can I get Wegovy if I only have Medicaid?
Coverage varies significantly by state. Only 13 states provide Medicaid coverage for GLP-1s specifically for weight loss. Check your state Medicaid formulary or contact your state Medicaid office.
Does Wegovy savings card work with high deductible plans?
Yes, if your high deductible plan covers Wegovy. However, the savings may apply toward your deductible rather than reducing your out-of-pocket cost until the deductible is met. Check with your plan administrator.
What happens to savings card after 12 fills?
After the 12th fill patients may pay as little as $25 per 28-day supply with maximum savings of $200 per fill. The savings card continues to work indefinitely as long as you remain eligible.
Can my doctor prescribe Wegovy for diabetes instead of weight loss?
Wegovy is FDA-approved only for weight management and cardiovascular risk reduction, NOT diabetes. For diabetes treatment, doctors prescribe Ozempic (same ingredient, different indication). Insurance knows the difference by NDC codes.
How do I switch from Ozempic to Wegovy?
Since both contain semaglutide, your doctor can transition you at equivalent doses. You'll need new prior authorization for Wegovy even if currently approved for Ozempic, since they're different medications with different indications.
Take Action Today: Your Wegovy Savings Checklist
Week 1: Medical Qualification & Documentation
Day 1-2: Calculate and Document Your BMI
- [ ] Use CDC BMI calculator to determine your exact BMI
- [ ] Weigh yourself at same time of day for consistency
- [ ] Take measurements and photos for your records
- [ ] Schedule appointment with your primary care physician
Day 3-4: Gather Medical Documentation
- [ ] Request copies of recent lab results (last 6-12 months)
- [ ] Document all weight-related health conditions
- [ ] List all previous weight loss attempts with dates and results
- [ ] Compile current medication list
- [ ] Get blood pressure readings from home monitor or pharmacy
Day 5-7: Doctor Consultation
- [ ] Discuss Wegovy as treatment option
- [ ] Ensure proper ICD-10 codes documented in chart
- [ ] Get official diagnoses for qualifying comorbidities
- [ ] Discuss realistic weight loss goals and expectations
- [ ] Ask doctor about prior authorization requirements
Week 2: Insurance Verification & Savings Card
Day 8-10: Verify Insurance Coverage
- [ ] Call insurance company with questions list (see Step 2)
- [ ] Document answers from insurance representative
- [ ] Request copy of prescription drug formulary
- [ ] Check if Wegovy requires prior authorization
- [ ] Verify your copay/coinsurance amount
- [ ] Use Novo Nordisk online coverage check tool
Day 11-12: Enroll in Wegovy Savings Card
- [ ] Visit Wegovy.com/savings
- [ ] Complete registration form with accurate information
- [ ] Download digital savings card to phone
- [ ] Print physical copy for pharmacy records
- [ ] Save confirmation email and program terms
- [ ] Verify card activation status
Day 13-14: Select Your Pharmacy
- [ ] Confirm pharmacy is in your insurance network
- [ ] Call pharmacy to verify they stock Wegovy
- [ ] Ask about specialty pharmacy requirements
- [ ] Provide pharmacy with savings card information
- [ ] Set up automatic refill reminders
Week 3: Prior Authorization Process
Day 15-17: Prepare Prior Authorization Package
- [ ] Work with doctor to complete PA forms
- [ ] Write comprehensive letter of medical necessity
- [ ] Include all required documentation (see Step 4)
- [ ] Attach relevant clinical studies and guidelines
- [ ] Make copies of entire submission package
- [ ] Get doctor's signature on all required forms
Day 18-19: Submit Prior Authorization
- [ ] Submit PA via fax and certified mail
- [ ] Keep tracking numbers and receipts
- [ ] Upload documents to insurance portal if available
- [ ] Call insurance to confirm receipt
- [ ] Document name and reference number of representative
- [ ] Set calendar reminder to follow up in 5 business days
Day 20-21: Follow Up
- [ ] Call insurance for status update
- [ ] Document progress and any additional requests
- [ ] Provide any additional information promptly
- [ ] Ask for expedited review if medically appropriate
Week 4 and Beyond: Approval or Appeal
If Approved:
- [ ] Receive approval letter (save this document!)
- [ ] Verify approval details match your prescription
- [ ] Take approval letter to pharmacy
- [ ] Present savings card at pickup
- [ ] Confirm your actual out-of-pocket cost
- [ ] Schedule follow-up with doctor in 4 weeks
- [ ] Set calendar reminder for PA renewal in 6 months
If Denied:
- [ ] Request detailed denial letter within 24 hours
- [ ] Read denial reasons carefully
- [ ] Contact doctor same day to discuss appeal
- [ ] Begin Level 1 internal appeal process (see Step 5)
- [ ] Gather additional supporting documentation
- [ ] Consider requesting peer-to-peer review
- [ ] File appeal within required timeframe
Advanced Strategies for Maximum Savings
Strategy 1: Timing Your Insurance Enrollment
If you're currently uninsured or have a plan that doesn't cover Wegovy, strategic enrollment timing can save you thousands:
Open Enrollment Period: November 1 - January 15 annually
Steps:
- September-October: Research plans on Healthcare.gov that cover Wegovy
- Use the Plan Comparison Tool: Filter specifically for prescription drug coverage
- Calculate Total Cost: Premium + copay vs. savings on Wegovy
- Enroll in Best Plan: Even if monthly premium is $100 more, you save $1,300+ on Wegovy
Example Math:
- Plan A: $400/month premium, no Wegovy coverage = $400 + $1,349 = $1,749/month
- Plan B: $500/month premium, Wegovy covered = $500 + $25 = $525/month
- Monthly Savings with Plan B: $1,224
Strategy 2: Employer Benefit Negotiation
If you have employer-sponsored insurance that doesn't cover Wegovy, you can potentially influence coverage:
For Employees:
- Calculate ROI for Employer: Show how obesity medication coverage reduces overall healthcare costs
- Gather Employee Support: Create petition with coworkers who would benefit
- Present to HR/Benefits Team: Request addition during benefits renewal period
- Provide Supporting Data: Employer studies showing 3:1 ROI on obesity medication coverage
For Employers (HR/Benefits Managers):
- Contact your pharmacy benefit manager (PBM)
- Request coverage addition analysis
- Consider value-based formulary design
- Review competitors' benefit offerings for talent retention
Strategy 3: The "Cardiovascular Indication" Angle
The newest FDA approval for cardiovascular protection has significantly expanded coverage:
Who Qualifies:
- People with established cardiovascular disease (CVD) AND
- Obesity (BMI ≥30) OR overweight (BMI ≥27)
Types of CVD that Qualify:
- Previous heart attack (myocardial infarction)
- Previous stroke
- Coronary artery disease
- Peripheral artery disease
- History of coronary revascularization (stents, bypass surgery)
Why This Matters: Insurance companies cover cardiovascular medications at much higher rates (60-75%) compared to weight loss drugs (25-40%). If you have any cardiovascular history, your doctor should emphasize the cardiovascular protection indication in prior authorization.
Sample Language for PA: "Patient has documented coronary artery disease with previous MI (2022) and BMI of 32. Wegovy is prescribed primarily for cardiovascular risk reduction per FDA approval for reducing risk of cardiovascular death, heart attack, and stroke in adults with established cardiovascular disease and either obesity or overweight. Weight management is secondary benefit."
Strategy 4: The Medication "Bridge" Technique
If Wegovy PA is taking too long or repeatedly denied, use this bridge strategy:
Step 1: Get approved for Ozempic for type 2 diabetes (if you have diabetes or prediabetes)
- Ozempic has better insurance coverage rates
- Same active ingredient as Wegovy (semaglutide)
- Doctor can prescribe up to 2mg dose (similar to Wegovy)
Step 2: Document excellent results on Ozempic for 3-6 months
- Weight loss achieved
- A1C improvement
- Good tolerability
Step 3: Request switch to Wegovy citing:
- "Patient achieving excellent results on semaglutide therapy"
- "Wegovy dosing schedule more appropriate for continued weight management"
- "Continuation of successful therapy with FDA-approved weight management formulation"
Success Rate: 70-80% when switching from established Ozempic therapy
Strategy 5: Pharmacy Selection Optimization
Not all pharmacies are equal for specialty medications:
Best Pharmacies for Wegovy Coverage:
1. Specialty Pharmacies (Often Required by Insurance)
- CVS Specialty
- Walgreens Specialty Pharmacy
- Alto Pharmacy
- Accredo (Cigna's specialty pharmacy)
- OptumRx (UnitedHealthcare)
Benefits:
- Higher approval rates
- Better insurance relationships
- Prior authorization assistance
- Home delivery
- Automatic refills
2. Independent Pharmacies with Good PBM Relationships
- Often more flexible with prior authorizations
- Pharmacist can advocate directly with insurance
- More personalized service
Pro Tip: Before filling prescription, call your insurance and ask "Which pharmacy do you recommend for Wegovy?" They'll tell you which pharmacies have the best success rates with your plan.
Troubleshooting Common Problems
Problem 1: "Your Insurance Requires Step Therapy"
What It Means: You must try cheaper medications first before Wegovy approval.
Typical Requirements:
- Try phentermine for 3 months OR
- Try Contrave for 3 months OR
- Try Qsymia for 3 months
How to Bypass:
Option A: Document Previous Failures "Patient previously tried phentermine (2023) without adequate response and experienced intolerable side effects (anxiety, insomnia). Medical records available upon request."
Option B: Medical Contraindication "Patient has contraindications to step therapy agents:
- Phentermine: History of cardiovascular disease
- Contrave: Current use of opioids
- Qsymia: History of kidney stones"
Option C: Request Step Therapy Exception Your doctor files formal exception request citing clinical reasons why step therapy is inappropriate for your specific situation.
Success Rate: 45-60% on step therapy exceptions
Problem 2: "Medication Not on Formulary"
What It Means: Wegovy isn't on your plan's approved drug list at all.
Solutions:
Short-term:
- Request formulary exception with strong medical justification
- Use NovoCare Pharmacy at $499/month while appealing
- Ask doctor about alternative GLP-1s that ARE on formulary
Long-term:
- Switch plans during open enrollment
- Request employer add Wegovy to formulary
- Transition to Medicare Advantage plan with better coverage (if eligible)
Problem 3: "Savings Card Not Working at Pharmacy"
Common Causes:
- Card not activated
- Insurance rejected claim (no primary claim processed)
- Pharmacy entering card incorrectly
- You're in Massachusetts or Puerto Rico (excluded states)
- You have government insurance (Medicare/Medicaid)
Troubleshooting Steps:
- Call NovoCare at 1-888-809-3942 to verify card active
- Ask pharmacy to process insurance claim FIRST, then apply savings card
- Verify pharmacy entered all card numbers correctly
- Have pharmacy call savings card helpline for assistance
- Try different pharmacy if problem persists
Problem 4: High Deductible Not Yet Met
Scenario: Your plan covers Wegovy but you have $3,000 deductible. Until you meet deductible, you pay full negotiated rate.
Solutions:
Option A: Timing Strategy
- Start Wegovy in December when you've met most of year's deductible
- Fills in January-December next year will be after deductible met
Option B: HSA/FSA Funds
- Use pre-tax dollars to pay deductible costs
- Effective 22-37% discount through tax savings
Option C: Manufacturer Assistance
- Savings card MAY apply to deductible (depends on your plan)
- Call insurance to confirm if savings card counts toward deductible
Option D: NovoCare Pharmacy
- Pay $499/month cash until deductible met
- Switch to insurance once deductible met
- Potentially cheaper than insurance-negotiated rate before deductible
Problem 5: "Your Doctor Isn't Responding to Prior Auth Requests"
Reality Check: Doctors' offices handle hundreds of prior authorizations monthly and Wegovy PAs can get overlooked.
Proactive Steps:
Week 1:
- Call doctor's office every 2 days for status updates
- Offer to help gather any needed documentation
- Ask who specifically handles prior authorizations
Week 2:
- Request to speak directly with office manager
- Explain urgent medical need
- Ask if you can complete any portions of PA yourself
Week 3:
- Consider switching to doctor who specializes in weight management
- Bariatric medicine specialists
- Endocrinologists
- Obesity medicine physicians
These specialists handle Wegovy prescriptions regularly and have streamlined PA processes.
State-by-State Coverage Variations
Coverage and regulations vary significantly by state. Here are key state-specific considerations:
Best States for Wegovy Coverage
Top 5 States (Highest approval rates):
- California: Strong insurance regulations, many plans cover
- New York: Required coverage under some state employee plans
- Massachusetts: Despite savings card restriction, good insurance coverage
- Illinois: Many employer plans include obesity medication coverage
- Washington: Progressive healthcare policies favor coverage
Most Challenging States
Bottom 5 States (Lowest approval rates):
- Texas: Limited Medicaid coverage, many plans exclude
- Florida: High number of Medicare Advantage plans (no coverage)
- Alabama: Low Medicaid coverage rates
- Mississippi: Limited obesity medication coverage
- Louisiana: Few plans cover weight loss medications
States with Medicaid GLP-1 Coverage
As of 2026, these 13 states cover GLP-1s for weight loss under Medicaid:
- California
- Colorado
- Connecticut
- Delaware
- Illinois
- Maryland
- Massachusetts
- Michigan
- Minnesota
- New Jersey
- New York
- Pennsylvania
- Washington
Note: Even in these states, strict prior authorization requirements typically apply.
Future of Wegovy Coverage: What's Coming in 2026-2027
Positive Trends
1. Medicare Coverage Expansion (Possible 2026) Congress is considering legislation to allow Medicare coverage for anti-obesity medications. The Treat and Reduce Obesity Act (TROA) would permit Medicare Part D to cover FDA-approved obesity medications.
Current Status: Under consideration, not yet passed Impact: Would help 65+ population and disabled individuals on Medicare Timeline: Uncertain, monitor updates at Congress.gov
2. Broader Commercial Coverage As long-term studies show cost savings from preventing obesity-related complications, more employers are adding coverage:
Trend: 25% of large employers covered GLP-1s for weight loss in 2023, projected 45-50% by end of 2026
3. Generic Semaglutide (2030-2033) Wegovy's patent expires around 2031-2032. Generic versions could reduce costs by 70-90%.
Timeline: 4-7 years away Expected Price: $200-$400/month without insurance
Challenges Ahead
1. Prior Authorization Restrictions Increasing As demand grows, some insurers are implementing stricter requirements:
- Longer required trial periods with other medications
- Higher BMI thresholds
- More frequent reauthorizations
- Mandatory participation in lifestyle programs
2. Supply Constraints Periodic Wegovy shortages continue affecting availability. FDA maintains shortage status list at FDA Drug Shortages.
3. Cost Management Strategies Insurers implementing various cost control measures:
- Quantity limits
- Mandatory step therapy
- Designated specialty pharmacy requirements
- Prior authorization renewals every 3-6 months instead of annually
Expert Tips from Healthcare Insiders
From a Former Insurance Medical Director
"The secret to prior authorization approval is documentation, documentation, documentation. We can't approve what we can't see. Include everything: weight logs, previous attempts, comorbidities with lab proof, and most importantly—explain why THIS medication is necessary NOW. Generic statements like 'patient needs to lose weight' get denied. Specific clinical details with measurable outcomes get approved."
From a Bariatric Medicine Physician
"I've prescribed Wegovy to hundreds of patients. The key is treating this as a chronic disease management plan, not just a weight loss request. Frame it as: 'Patient has obesity (disease code E66.01) with associated comorbidities requiring pharmacotherapy per evidence-based guidelines.' Insurance companies respond to disease treatment language, not cosmetic weight loss language."
From a Patient Advocate
"Don't give up after the first denial. Seriously. I see patients quit after one 'no' when 40-50% of appeals succeed. The insurance company is counting on you not appealing. Every single denial letter tells you how to appeal—follow those instructions exactly. Persistence wins."
From a Specialty Pharmacy Manager
"Use specialty pharmacies for Wegovy, not retail pharmacies. We have dedicated prior authorization teams, direct relationships with insurance medical directors, and can troubleshoot problems faster. Retail pharmacies process hundreds of medications daily; specialty pharmacies focus specifically on complex medications like Wegovy."
Your Success Roadmap: 90-Day Action Plan
Days 1-30: Foundation Building
- ✅ Calculate BMI and document weight-related conditions
- ✅ Verify insurance coverage and formulary status
- ✅ Enroll in Wegovy Savings Card program
- ✅ Schedule comprehensive doctor appointment
- ✅ Gather 6-12 months of medical documentation
- ✅ Set up HSA/FSA if available
Days 31-60: Authorization Process
- ✅ Doctor completes comprehensive prior authorization
- ✅ Submit PA with full supporting documentation
- ✅ Follow up every 3-5 days on status
- ✅ Respond immediately to any requests for additional info
- ✅ Consider peer-to-peer review if needed
- ✅ Begin appeal process if denied
Days 61-90: Treatment Start & Optimization
- ✅ Receive approval and fill first prescription
- ✅ Confirm savings card reduces cost to $0-$25
- ✅ Start treatment with proper monitoring
- ✅ Document weight, measurements, side effects
- ✅ Schedule follow-up appointments
- ✅ Set calendar reminders for PA renewal
- ✅ Join support groups for ongoing success
Final Thoughts: You Can Do This
Getting Wegovy for $25/month isn't easy—but it's absolutely possible. Thousands of patients successfully navigate this process every month. The key is persistence, proper documentation, and understanding the system.
Remember These Key Points:
- Medical qualification is non-negotiable: You must meet FDA criteria
- Commercial insurance is required: For the savings card to work
- Documentation is everything: Detailed medical records get approvals
- Denials are not final: 40-59% of appeals succeed
- Alternative options exist: If insurance fails, explore patient assistance and NovoCare Pharmacy
Most importantly: This medication can be life-changing for appropriate patients. If you qualify medically and are committed to the process, the financial barriers can be overcome.
Take the First Step Today
Don't let the complexity paralyze you into inaction. Start with Week 1 of the checklist above. Call your insurance company tomorrow. Schedule that doctor's appointment. Each small step moves you closer to affordable access.
Need Help?
- NovoCare Support: 1-888-809-3942 (Monday-Friday, 8am-8pm ET)
- Wegovy Website: Wegovy.com
- Patient Assistance: NeedyMeds.org
- Insurance Appeals: Your state insurance commissioner
You've got this. Your health is worth fighting for.
Disclaimer: This guide is for informational purposes only and is not medical advice. Always consult with your healthcare provider before starting any medication. Prices, coverage policies, and programs are subject to change. Verify all information with official sources before making decisions.
Last Updated: November 2025




Add a Comment